Emergency Dental Services in Portland, OR
Most Dental Emergencies Can’t Wait – We are committed to seeing you today! Call Us Now for Emergency Dental Care!
Dental emergencies happen at random and can affect your ability to carry out your daily routine. At On Q in Portland, we understand that emergencies are uncontrollable, which is why we offer extended morning and weekend hours. Our Portland, OR office works around busy schedules just like yours so that you can receive the dental care you need. We also offer easy payment options, financing, and savings plans in order to expedite your emergency dental care.
A dental emergency service can include any of the following:
- Fractured or broken tooth
- Severe toothache
- Broken filling
- Unexplained tooth loss
- Painful, bleeding, or swollen gums
Do not hesitate to call our Portland, OR office if you are experiencing a dental emergency. We are dedicated to providing thorough and immediate care so that you can get back on track.
The most important step is to contact your Portland, OR dental office and schedule an appointment immediately. There is no reason to wait when you are experiencing discomfort and pain. The longer an emergency goes without being treated, the more likely it is that an infection will grow. Before the pain and discomfort get worse, call us today and get your dental emergency service taken care of!
If you have a tooth that’s been knocked out, there are certain steps you can take before you come to our office:
To preserve the tissues around the tooth root, place the tooth back in your mouth where it fell out. Bite down on it using gauze or a wet tea bag to keep the tooth in place.
For a displaced tooth, place the tooth in a container and cover it with a little whole milk or saliva. If your tooth has not fully detached, the tooth is between your lower gums and lower lip.
You can also hold your tooth underneath your tongue.
Use a tooth-saving storage container, which will include a fluid solution.
Be sure to save the tooth that has been knocked out and bring it to your dentist immediately. Do not handle the tooth by the root, or attempt to brush or clean it using solutions like rubbing alcohol or hydrogen peroxide, and most importantly, DO NOT WAIT to call us.
It is also important not to scratch the tooth, which is why we suggest holding it in a container or in your mouth.
In the past, if you had a tooth with a diseased nerve, you’d probably lose that tooth. Now, with “root canal therapy,” your tooth can be saved. When a tooth is cracked or has a deep cavity, bacteria can enter the pulp tissue and germs can cause an infection inside the tooth. If left untreated, an abscess may form. If the infected tissue is not removed, pain and swelling can result. This can injure your jawbones and be harmful to your overall health.
Root canal therapy involves one to three visits. During treatment, your general dentist or endodontist removes the affected tissue. Next, the interior of the tooth will be cleaned and sealed. Finally, the tooth is filled with a dental composite. If your tooth has extensive decay, your dentist may suggest placing a crown to strengthen and protect the tooth from breaking. As long as you continue to care for your teeth and gums with regular brushing, flossing, and checkups, your restored tooth can last a lifetime.
What is a root canal procedure?
Tooth decay can progress down into the pulp. When this happens, the pulp can become infected. Infection of the pulp can be very painful and can also deteriorate into an abscessed tooth when infection and swelling develop in the tissues around or beneath the tooth. When the pulp becomes infected or the tooth becomes abscessed, it is necessary to perform a root canal.
Why do I feel pain?
When the pulp becomes infected due to a deep cavity or fracture, bacteria can seep in. When there has been an injury due to trauma, the pulp can die. Damaged or dead pulp causes increased blood flow, pressure, and cellular activity. Pain in the tooth is commonly felt when biting down or chewing, and eating or drinking hot and/or cold foods and beverages.
Why do I need root canal therapy?
The tooth will not heal by itself. Without treatment, the infection will spread. The bone around the tooth will begin to degenerate, and the tooth may fall out. The pain usually worsens until one is forced to seek emergency dental attention. The only alternative is extraction of the tooth, which can cause the surrounding teeth to shift, resulting in a bad bite. Though an extraction is cheaper, the space left behind will require an implant or a bridge, which can be more expensive than root canal therapy. If you have the choice, it’s always best to keep your original teeth.
What are the risks and complications of root canal therapy?
More than 95 percent of root canal therapies are successful. However, sometimes a case needs to be redone due to diseased canal offshoots that went undetected, or the fracturing of the canal filling. More commonly, root canal therapy will fail altogether, marked by the return of pain.
What happens after root canal therapy?
Once root canal therapy is completed, the endodontist will refer the patient back to our office for the permanent restoration of the tooth. A temporary filling was placed immediately following the root canal therapy and will need to be replaced with a permanent filling or crown and build-up. A crown will be necessary on all posterior teeth to properly protect the root canal-treated tooth from fracturing. Front teeth can typically be restored with a filling, however a crown may be necessary in some cases. Your dentist will determine the best choice for your individual needs.
How long will the restored tooth last?
Your restored tooth could last a lifetime, if you continue to care for your teeth and gums. However, regular checkups are necessary. As long as the root(s) of a treated tooth are nourished by the tissues around it, your tooth will remain healthy.
How does root canal therapy save my tooth?
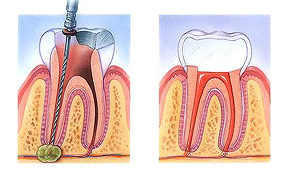
- An opening is made through the crown of the tooth and entered the pulp chamber.
- The pulp is removed, and the root canals are cleaned, enlarged, and shaped.
- Medications may be put in the pulp chamber and root canal(s) to help get rid of germs and prevent infection.
- A temporary filling will be placed in the crown opening to protect the tooth between dental visits. Your dentist may leave the tooth open for a few days to drain. You might also be given medicine to help control infection that may have spread beyond the tooth.
- The temporary filling is removed and the pulp chamber and root canal(s) are cleaned and filled.
- In the final step, a gold or porcelain crown is usually placed over the tooth.
An infected tooth is a serious condition and must be treated promptly to avoid tooth loss and the spreading of infection to other teeth. If you are concerned about an infected or abscessed tooth, we urge you to contact us promptly.
When patients experience extreme sensitivity, or pain from a broken tooth, or are suffering from advanced periodontal disease, your dentist could recommend that they have a tooth extracted. During a simple extraction, the dentist can safely remove the affected tooth without the need for major surgery.
Reasons for Tooth Extractions
There are numerous situations in which a simple extraction is needed. Extractions are typically performed because of an active problem such as pain, swelling, decay, or infection, as a preventative measure to avoid serious problems in the future or to prepare you for another cosmetic or restorative procedure.
Common reasons for tooth extractions include:
- Advanced periodontal disease that has loosened the roots of your tooth
- Extra teeth or baby teeth that impede adult teeth
- Preparing a patient for orthodontic treatment
- Removing a fractured or malformed tooth
- Severe tooth decay which cannot be remedied with root canal therapy
- Removal of Wisdom Teeth
How Tooth Extractions Are Done
Although we often hope to avoid the extraction of a tooth, sometimes it is necessary if the tooth cannot be saved by a root canal or other dental procedure.
Extractions are usually performed under local anesthesia.
Once the tooth has been pulled, a blood clot will form in the socket. The dentist will place a few stitches (usually dissolvable sutures) to close the gums over the extraction site. The dentist will pack a gauze pad into the socket and have you bite down on it. This will help stop the bleeding and help the clot form. It’s important to let the clot heal and form properly. If the blood clot does not form properly, you can run the risk of a painful condition called dry socket.
Home Care Instructions for Tooth Extractions
It normally takes several days to recover from an extraction. You will be placed on a soft food diet for several days, need rest limit strenuous activity, and refrain from smoking, rinsing, and using straws.
Next Step – Schedule An Appointment
Our dental team will work to save your tooth first but will provide the necessary care and attention needed if an extraction is required. Call our office today for an appointment and a treatment plan for an extraction.
While not all wisdom teeth require removal, wisdom teeth extractions are most often performed because of an active problem such as pain, swelling, decay, or infection, or as a preventative measure to avoid serious problems in the future. If the impaction of one or more wisdom teeth is present and left untreated, a number of potentially harmful outcomes can occur.
What Are Wisdom Teeth
Third molars, commonly referred to as wisdom teeth, are usually the last four of 32 teeth to erupt (surface) in the mouth. Wisdom teeth generally make their appearance between the ages of 17 to 25. They are located at the back of the mouth (top and bottom), near the entrance to the throat. The term “wisdom” stems from the idea that the molars surface at a time typically associated with increased maturity or “wisdom”.
In most cases, inadequate space in the mouth does not allow the wisdom teeth to erupt properly and become fully functional. When this happens, the tooth can become impacted (stuck) in an undesirable or potentially harmful position. If left untreated, impacted wisdom teeth can contribute to infection, damage to other teeth, and possibly cysts or tumors.
There are several types, or degrees, of impaction, based on the actual depth of the teeth within the jaw:
- Soft Tissue Impaction: The upper portion of the tooth (the crown) has penetrated through the bone, but the gingiva (gum) is covering part or all of the tooth’s crown and has not positioned properly around the tooth. Because it is difficult to keep the area clean, food can become trapped below the gum and cause an infection and/or tooth decay, resulting in pain and swelling.
- Partial Bony Impaction: The tooth has partially erupted, but a portion of the crown remains submerged below the gum and surrounding jawbone. Again, because it is difficult to keep the area clean, infection will commonly occur.
- Complete Bony Impaction: The tooth is completely encased by the jawbone. This will require more complex removal techniques.
Reasons to Remove Your Wisdom Teeth
While not all wisdom teeth require removal, wisdom teeth extractions are most often performed because of an active problem such as pain, swelling, decay, or infection, or as a preventative measure to avoid serious problems in the future. If impaction of one or more wisdom teeth is present and left untreated, a number of potentially harmful outcomes can occur, including:
- Damage to nearby teeth: Second molars (the teeth directly in front of the wisdom teeth) can be adversely affected by impacted wisdom teeth, resulting in tooth decay (cavities), periodontal disease (gum disease), and possible bone loss.
- Disease: Although uncommon, cysts and tumors can occur in the areas surrounding impacted wisdom teeth.
- Infection: Bacteria and food can become trapped under the gum tissue, resulting in an infection. The infection can cause considerable pain and danger.
- Tooth Crowding: It has been theorized that impacted wisdom teeth can put pressure on other teeth and cause them to become misaligned (crowded or twisted). This theory isn’t universally accepted by all dental professionals, and it has never been validated by any scientific studies.
Wisdom Teeth Examination
As with any dental procedure, your dentist will want to initially conduct a thorough examination of the wisdom and surrounding teeth. Panoramic or digital X-rays will be taken in order for your dentist to evaluate the position of the wisdom teeth and determine if a current problem exists, or the likelihood of any potential future problems. The X-rays can also expose additional risk factors, such as deterioration or decay of nearby teeth. Early evaluation and treatment (typically in the mid-teen years) are recommended in order to identify potential problems and to improve the results for patients requiring wisdom teeth extractions. Only after a thorough examination can your dentist provide you with the best options for your particular case.
What Does The Removal of Wisdom Teeth Involve?
Wisdom teeth removal is a common procedure, generally performed under local anesthesia, intravenous (IV) sedation, or general anesthesia by a specially trained dentist, in an office surgery suite. The surgery does not require an overnight stay, and you will be released with post-operative instructions and medication (if necessary) to help manage any swelling or discomfort.
Aftercare For Wisdom Teeth Extractions
Your dentist will give you take-home instructions on how to care for the surgical sites, precautions during the healing process, what to expect, and other information.
If you experience any issues or discomfort following your procedure, please contact our office as soon as possible.
Get Your Wisdom Teeth Removed
Are your wisdom teeth causing you pain, or do you think you’re a candidate to have them removed? Call our office today for a consultation.